Last week, I posted a ‘miniband hack’ video for quadriceps strengthening on my Instagram account (without making any tremendously bold claims…or so I thought) and got a lot of really interesting responses and reactions from various rehabilitation specialists around the world. While my page has a large following of clinicians, it was specifically designed for soccer players and coaches, so I will try to meet you all on a middle ground during this blog post. At the risk of over-simplifying an important rehabilitation concept, I will walk you through my thought-process regarding the heavily scrutinized topic of whether open-kinetic chain (OKC) quadriceps strengthening is appropriate in the athlete recovering from ACL reconstruction.

Before we get into it, I would like to provide the disclaimer that I am not right, and you are not wrong. Much like today’s political climate, there seems to be a huge polarity between practitioners who support OKC strengthening and those who do not. Regardless of which side of the fence you sit, I challenge you to open your mind for the next ten minutes. Turn autopilot off and let’s review the facts.

First, let’s start with the difference between closed-kinetic chain (CKC) and open-kinetic chain exercise. In CKC exercise, the distal segment of the lower extremity (the tibia, or the “shin bone”) is fixed/stabilized to the ground. This means that you are in a weight bearing (WB) position performing tasks like the squat, lunge, or step-up. Clinicians may choose to implement CKC exercises because they are ‘functional.’ We do these types of movements everyday. CKC exercises also increase joint congruency and compressive forces, decrease shear and acceleration forces, stimulate proprioceptors, and enhance dynamic stability, neuromuscular control, and balance. Co-contraction of agonist and antagonist muscles helps to provide joint stability, thereby decreasing shear forces that can jeopardize surrounding soft tissues.
Essentially, all this means is that during CKC lower extremity exercise, you get firing of the muscles on both sides of the leg (i.e. the quads and the hamstrings), resulting in less stress or strain to healing structures (i.e. that newly reconstructed ACL).

In OKC exercise, the distal segment of the joint is moving. These are typically non-weight-bearing (NWB) exercises like knee extensions. With knee extensions, the shin bone is moving on a fixed thigh bone. OKC exercises can isolate a single muscle group and are extremely beneficial from a strengthening and range of motion (ROM) standpoint, as they can correct strength deficits that may be difficult to address during WB activities. However, OKC exercise does have its fair share of disadvantages, as there are typically increased acceleration forces, increased distraction and rotational forces, increased deformation of joint and muscle mechanoreceptors, as well as greater moment arms and shear forces to healing structures.

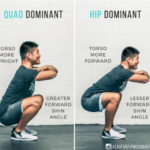
We know that, on average, ACLR patients show a 28.5% decrease in quadriceps strength relative to the uninvolved leg at 7.5 months post-op due to diminished motoneuron recruitment and decreased motor-unit-firing frequency. Perhaps this is due to the ever-frequent compensatory strategies we see in ACLR patients during CKC exercise. Roos et al. (2014) found that even at 13 months post ACLR, individuals tend to exhibit average knee extensor moments that are 17% smaller in the surgical limb compared to the nonsurgical limb during a simple bodyweight squat. Sigward et al. (2018) found that recovering athletes tend to implement two specific compensatory strategies, often without even realizing it. These researchers found that at the 3-month mark, patients often utilize an ‘interlimb’ compensation pattern, meaning that they often shift their weight onto the nonoperative leg, allowing the ‘good’ leg to do most of the work. Interestingly enough, these researchers found a different ‘intralimb’ compensation strategy at the 5-month mark where, although patients were bearing equal weight through each leg, they were implementing a hip-dominant squat strategy to reduce demands on the quads. Both compensation patterns may be elicited subconsciously, preventing a recovering athlete from effectively strengthening his or her quads during rehabilitation. This can unfortunately come back to haunt the athlete, as Grindem et al. (2016) showed that for every 1% decrease in quadriceps strength relative to 90% of the opposite side, risk of knee re-injury increases by as much as 3%. This not only includes ACL injury, but other serious ligamentous and cartilaginous pathologies as well.
(Left) Asymmetrical interlimb compensation strategy. (Right) Hip dominant intralimb compensation strategy.
Now that we have discussed the prevalence of quadriceps weakness following ACLR and the various compensation patterns seen in CKC exercise, let’s talk about why OKC quadriceps strengthening often makes clinicians sweat…
During OKC quadriceps strengthening, the knee starts from a NWB flexed position and extends out straight. If you recall back to that musculoskeletal lecture in PT school, the knee follows the “concave on convex” rule, where the tibia both rolls and glides anteriorly on the femur. Wait – isn’t this exactly what the ACL prevents!? Yes. The ACL prevents anterior translation of the tibia on the femur in open-kinetic chain. The ACL also prevents posterior translation of the femur on the tibia in closed-kinetic chain. Plot twist: This means that you stress the ACL during both OKC and CKC exercise.

It is a well-accepted fact in the rehabilitation community that anterior shear forces to the ACL are greatest anywhere from 0 to 30 degrees of knee flexion in both NWB and WB positions. These forces gradually decrease between 30 and 60 degrees of knee flexion, and are essentially non-existent at flexion angles greater than 60 degrees. For this reason, many physical therapists and other sports medicine clinicians alike avoid terminal knee extension in open-kinetic chain for up to 1 year post-surgery. Short-arc quads, and long-arc quads for that matter, are often left to the wayside as an athlete progresses through rehabilitation.
Could we possibly be doing our patients a disservice by excluding exercises that so clearly and efficiently strengthen the quadriceps musculature?

I recently partook in Mike Reinold and Lenny Macrina’s Master Course on Knee Evaluation and Treatment. During this course, ACL peak strain percentage was discussed in both WB and NWB exercises, as well as during different points in the ROM. My inner nerd was intrigued, so I decided to do a little bit more digging. After reading various articles like Escamilla et al. (2012) and Beynnon et al. (1997), I found myself reviewing the numbers:

(Above) Beynnon & Fleming (1998). Anterior cruciate ligament strain in-vivo: A review of previous work.

(Above) Escamilla et al. (2012). Anterior Cruciate Ligament Strain and Tensile Forces for Weight-Bearing and Non–Weight-Bearing Exercises: A Guide to Exercise Selection.
Okay, so what does all of this mean? I’d like to draw your attention to ACL strain produced during body weight squatting and squatting with a 30-pound sport cord. ACL strain is anywhere between 3.6-4.0%. Now, let’s look at ACL strain during dynamic seated knee extension with and without 10-pounds of resistance. ACL strain is anywhere between 2.8 and 3.8%. If you are a clinician who loads up the goblet squat, sumo squat, front or back barbell squat, and you do not include open-chain knee extensions, I pose the question to you: why not?

The similarity of ACL strain during these two frequently prescribed rehabilitation exercises calls into question the appropriateness of deeming exercises ‘safe’ or ‘unsafe’ simply on the premise of them being open or closed-kinetic chain. If you exclude simple knee flexion-extension AROM from your plan of care, shouldn’t you also be excluding single-leg sit to stands, single-leg squatting, and stair climbing? Let’s hope your patient doesn’t have a flight of stairs or two in his/her home.
Escamilla et al. also describes the peak anterior shear force (in Newtons) and corresponding knee angle for WB and NWB exercises. Did you know that level-ground walking produces approximately 355 N of anterior shear force when the knee of the WB limb is in approximately 15 to 20 degrees of knee flexion as the opposite foot approaches toe-off? Similarly, Wilk & Andrews found that peak ACL loading during a 0 to 90 degree dynamic seated knee extension for 12 repetitions of maximal resistance produced approximately 248 N of anterior shear force. Though gait training is deemed more functional in this sense than dynamic knee extensions during early rehabilitation, you can see what I’m getting at here…

While the literature is currently mixed and exact ACL strain-to-failure is unknown, it is postulated that approximately 20-40% ligament strain will result in graft rupture (Reinold & Macrina, 2019). With most rehabilitation activities ranging anywhere from 2-4%, you can sleep easy knowing your patient is working at levels anywhere from 1/10th to 1/5th of these dangerous values when performing OKC knee extensions.

Now, I’m not telling you to jump off of the surgical table and start performing heavily-resisted unrestricted OKC knee extensions. If this type of strengthening is initiated too early, at improper knee angles, or at inappropriate load, you do risk increased laxity of your newly reconstructed ligament. You can now pump your fists, OKC haters of the world!
In a study by Heijne & Werner in 2007, researchers found that early introduction of NWB exercises (at 4 weeks versus 12 weeks) significantly increased anterior knee laxity and did not result in clinically significant strength gains. Here, OKC knee extensions were initiated at the 4-week mark, with 0 to 90 degree ROM achieved by weeks 5-6 and external resistance added to patient tolerance. Of note is the two types of graft used in this study – patellar tendon BTB and hamstring STG autograft. Though based on limited evidence, it is postulated that hamstring grafts are more susceptible to stretch and increased laxity than patellar tendon autografts due to different collagenous properties. The Heijne & Werner study showed that when OKC strengthening was initiated at the 4-week mark in patellar tendon BTB autografts, it resulted in no further increase in anterior laxity when compared to OKC initiated at the 12-week mark. Hamstring autografts were a different story, however, as OKC strengthening initiated at the 4-week mark resulted in significantly more anterior laxity when compared to OKC initiated at the 12-week mark.

Unlike Heijne & Werner, who progressed patients to unrestricted OKC ROM by week 6, Fukuda et al. (2013) implemented a supervised OKC exercise program starting at post-operative week 4. In that trial, the knee was mechanically locked between 90 and 45 degrees of knee flexion until 12 weeks post surgery, allowing for isolation of the quadriceps musculature and mitigation of ACL tensile strain. What they found was no difference in terms of anterior knee laxity when comparing OKC exercise initiated in a limited ROM at the 4-week mark versus unrestricted OKC strengthening at the 12-week mark.They did, however, find that early initiation of such exercise in the dose of 3 sets of 10 repetitions at 70% 1RM lead to a significant increases in quadriceps muscle strength at the 19-week, 25-week, and 17-month mark. Since the ACL graft undergoes significant remodeling and necrosis during the first 6 to 8 weeks following surgery (and a process called ‘ligamentization’ for up to 1 year post-op), Fukuda et al. also postulated that limiting ROM from 90 to 45 degrees early on can help prevent increases in anterior knee laxity.
Other studies refuting Heijne & Werner’s work include that of Tagesson et al. (2008) and Mikkelsen et al. (2000). Tagesson et al. compared early OKC exercise versus CKC exercise in post-operative ACL patients and found that those who performed OKC exercise demonstrated significantly greater isokinetic quadriceps strength with no other functional differences in joint laxity noted between the two groups. Similarly, Mikkelsen et al. showed that the addition of OKC quadriceps training 6 weeks after ACL reconstruction resulted in significantly greater quadriceps torque without reducing knee joint stability at the 6-month mark. Mikkelsen et al. also concluded that incorporating OKC exercise lead to a significantly higher number of athletes returning to their previous activity earlier and at their same pre-injury competitive level.

Well, when is it okay to start initiating these exercises? When can we progress to full ROM? When can we start to load the joint? While 79% of the 200+ clinicians polled on my IG last week said that OKC strengthening is appropriate following ACL reconstruction, there was a huge grey area regarding specific parameters. There is a large paucity in the literature regarding ideal timing of initiating OKC exercise, as well as appropriate restrictions regarding ROM and joint loading. There is also no definitive understanding of how graft type and/or patient population might play a role in the decision to include or exclude OKC exercise from your plan of care.
The Royal Dutch Society for Physical Therapy (KNGF) instructed a multidisciplinary group of ACL experts to develop a consensus statement for rehabilitation following ACL reconstruction. In August 2016, they released their evidence-based clinical practice update in the British Journal of Sports Medicine, stating that both OKC and CKC exercises are appropriate means of quadriceps strengthening following ACLR, and that OKC strengthening is safe to perform in a limited 45-90 degree ROM starting at 4 weeks post-surgery. The authors failed to describe when these parameters should be lifted however, leaving ROM and external resistance judgment up to healthcare clinicians. Months prior to the publication of this update, the MOON Group (a collection of orthopaedic surgeons and their designated physical therapy committee) released their own evidence-based rehabilitation guidelines. These clinicians declared that OKC activities initiated after 6 weeks post-surgery may improve strength without adversely affecting the graft and/or increasing graft laxity. They also stated that the evidence regarding safety of such exercises before 6 weeks post-surgery is insufficient, requiring additional research be completed in this domain.

So…what’s the verdict? Unfortunately, I don’t have a “cookie-cutter” response for you. Professionally, I believe that in order to provide athletes with comprehensive and complete rehabilitation, we need to include both CKC and OKC quadriceps strengthening. We must understand each athlete’s individual presentation, taking into account his/her concomitant injuries and graft type, while also considering evidence-based practice guidelines and our own clinical judgements. As clinicians, we must continue to move our profession forward by staying current with the literature and by always challenging our implicit and explicit biases. I will say that for my own most recent ACL reconstruction, I initiated lightly-resisted 90-45’s at the 4-week mark and progressed to unrestricted OKC terminal knee extension at the 12-week mark. I evaluated the literature to the best of my ability and made an informed decision using my clinical judgment. What do you do with your patients? Please feel free to comment below, send me a private e-mail, or slide into my DM’s, and let’s keep this discussion going! Until next time, be well.
References
- Johnson AK, Palmieri-Smith RM, Lepley LK (2018) Contribution of neuromuscular factors to quadriceps asymmetry after anterior cruciate ligament reconstruction. J Athl Train 53:347–354
- Roos PE, Button K, van Deursen RW. Motor control strategies during double leg squat following anterior cruciate ligament rupture and reconstruction: an observational study.J Neuroeng Rehabil. 2014;11:19. https://doi. org/10.1186/1743-0003-11-19
- Sigward, S. M., Chan, M. M., Lin, P. E., Almansouri, S. Y., & Pratt, K. A. (2018). Compensatory Strategies That Reduce Knee Extensor Demand During a Bilateral Squat Change From 3 to 5 Months Following Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther, 48(9), 713-718. doi:10.2519/jospt.2018.7977
- Grindem H, Snyder-Mackler L, Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 2016; 50: 804–808.
- Mike Reinold and Lenny Macrina’s Online Master Class on Evaluation and Treatment of the Knee. 2019.
- Escamilla RF, Macleod TD, Wilk KE, Paulos L, Andrews JR. Anterior cruciate ligament strain and tensile forces for weight-bearing and non-weight-bearing exercises: a guide to exercise selection. J Orthop Sports Phys Ther. 2012;42(3):208–220.
- Beynnon, B. D., Johnson, R. J., Fleming, B. C., Stankewich, C. J., Renström, P. A., & Nichols, C. E. (1997). The Strain Behavior of the Anterior Cruciate Ligament During Squatting and Active Flexion-Extension: A Comparison of an Open and a Closed Kinetic Chain Exercise. The American Journal of Sports Medicine, 25(6), 823–829. https://doi.org/10.1177/036354659702500616
- Beynnon BD, Fleming BC (1998) Anterior cruciate ligament strain in-vivo: a review of previous work. J Biomech 31:519–525
- Nagura T, Matsumoto H, Kiriyama Y, Chaudhari A, Andriacchi TP. Tibiofemoral joint contact force in deep knee flexion and its consideration in knee osteoarthritis and joint replacement. J Appl Biomech. 2006;22:305-313.
- Wilk K E, Andrews J R. The effects of pad placement and angular velocity on tibial displacement during isokinetic exercise. J Orthop Sports Phys Ther. 1993;17:24–30.
- Hughes M. Why quads matter in ACL rehabilitation. Premax. 21 September 2018. Retrieved from https://www.premax.co/au/blog/why-quads-matter-in-acl-rehabilitation. Accessed 11 April 2019.
- Heijne A, Werner S. Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Knee Surg Sports Traumatol Arthrosc. 2007;15:402-414. http://dx.doi. org/10.1007/s00167-006-0246-z
- Perriman, A., Leahy, E., & Semciw, A. I. (2018). The Effect of Open- Versus Closed-Kinetic-Chain Exercises on Anterior Tibial Laxity, Strength, and Function Following Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. J Orthop Sports Phys Ther, 48(7), 552-566. doi:10.2519/jospt.2018.765
- Fukuda, T. Y., Fingerhut, D., Moreira, V. C., Camarini, P. M., Scodeller, N. F., Duarte, A., Jr., . . . Bryk, F. F. (2013). Open kinetic chain exercises in a restricted range of motion after anterior cruciate ligament reconstruction: a randomized controlled clinical trial. Am J Sports Med, 41(4), 788-794. doi:10.1177/0363546513476482
- Tagesson S, Oberg B, Good L, Kvist J. A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: a randomized clinical trial evaluating dynamic tibial translation and muscle function. Am J Sports Med. 2008;36:298-307. http://dx.doi. org/10.1177/0363546507307
- Mikkelsen C Werner S Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:337–42.
- van Melick, N., van Cingel, R. E., Brooijmans, F., Neeter, C., van Tienen, T., Hullegie, W., & Nijhuis-van der Sanden, M. W. (2016). Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med, 50(24), 1506-1515. doi:10.1136/bjsports-2015-095898
- Wright, R. W., Haas, A. K., Anderson, J., Calabrese, G., Cavanaugh, J., Hewett, T. E., . Williams, G. (2015). Anterior Cruciate Ligament Reconstruction Rehabilitation: MOON Guidelines. Sports Health, 7(3), 239-243. doi:10.1177/1941738113517855